Modelos para el estudio de las interacciones placenta-patógeno en parásitos apicomplejos

 La neosporosis bovina y la toxoplasmosis ovina son dos enfermedades parasitarias que causan importantes pérdidas económicas en el sector ganadero debido al fallo reproductivo que ocasionan.
La neosporosis bovina y la toxoplasmosis ovina son dos enfermedades parasitarias que causan importantes pérdidas económicas en el sector ganadero debido al fallo reproductivo que ocasionan.
 Estas enfermedades están causadas por Neospora caninum y Toxoplasma gondii, respectivamente, ambos son parásitos apicomplejos formadores de quistes estrechamente relacionados, y que comparten muchas características morfológicas y biológicas24,25.
Estas enfermedades están causadas por Neospora caninum y Toxoplasma gondii, respectivamente, ambos son parásitos apicomplejos formadores de quistes estrechamente relacionados, y que comparten muchas características morfológicas y biológicas24,25.
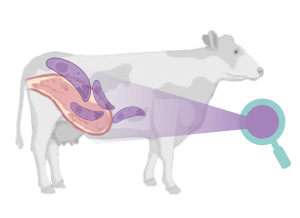
 La neosporosis bovina tiene una gran importancia en el ganado vacuno, ya que es una de las principales causas de aborto a nivel mundial, originando graves pérdidas económicas. El aborto es el principal signo clínico de la neosporosis bovina.
La neosporosis bovina tiene una gran importancia en el ganado vacuno, ya que es una de las principales causas de aborto a nivel mundial, originando graves pérdidas económicas. El aborto es el principal signo clínico de la neosporosis bovina.
![]() Los fetos de las madres infectadas por N. caninum pueden morir en el útero y ser reabsorbidos, momificados, sufrir autolisis o nacer muertos.
Los fetos de las madres infectadas por N. caninum pueden morir en el útero y ser reabsorbidos, momificados, sufrir autolisis o nacer muertos.
![]() Las vacas de cualquier edad pueden abortar desde los 3 meses de gestación hasta su término, observándose la mayoría de los abortos a los 5-7 meses de gestación21.
Las vacas de cualquier edad pueden abortar desde los 3 meses de gestación hasta su término, observándose la mayoría de los abortos a los 5-7 meses de gestación21.
![]() Si la infección ocurre después de la mitad de la gestación pueden nacer terneros vivos con signos clínicos o clínicamente normales, pero persistentemente infectados.
Si la infección ocurre después de la mitad de la gestación pueden nacer terneros vivos con signos clínicos o clínicamente normales, pero persistentemente infectados.
![]() El fallo reproductivo puede producirse también en otros rumiantes como ovejas, cabras y ciervos21,26,27.
El fallo reproductivo puede producirse también en otros rumiantes como ovejas, cabras y ciervos21,26,27.
 En la actualidad, no existen vacunas ni tratamientos eficaces contra la infección por N. caninum28,29 y las opciones de control se basan en el diagnóstico y en medidas de bioseguridad y manejo21. En la actualidad, no existen vacunas ni tratamientos eficaces contra la infección por N. caninum28,29 y las opciones de control se basan en el diagnóstico y en medidas de bioseguridad y manejo21. |
Por otro lado, la toxoplasmosis se considera una de las principales causas de pérdidas reproductivas en ovejas y cabras en todo el mundo22,30.
La infección durante la gestación suele provocar






 Latinoamérica
Latinoamérica Europa
Europa